Mental Health Crisis Among Youth: Why Early Intervention Matters

Mental Health Crisis Among Youth: Why Early Intervention Matters – Picture this: A 15-year-old honor student smiles through class, aces her tests, then goes home and cuts herself in secret.
A star athlete posts gym selfies with #Blessed captions, while privately battling paralyzing panic attacks before games.
A college freshman scrolls through Instagram at 3 AM, convinced everyone’s life is perfect except his.
This isn’t just teenage angst—it’s a full-blown mental health crisis.
Depression rates among teens doubled from 2009 to 2019. Emergency room visits for youth suicide attempts rose 51% in the pandemic’s first year. And here’s the gut punch: Half of all mental illnesses start by age 14.
We’re failing our kids. But there’s hope—if we act NOW.
The Numbers Don’t Lie: Youth Mental Health By the Stats
Let’s hit you with the hard data:
-
1 in 3 college students experiences significant depression
-
40% surge in adolescent depression since 2010
-
Suicide is now the second-leading cause of death for 10-24 year olds
But here’s what the stats DON’T show:
The honor student terrified she’ll disappoint her parents.
The class clown using jokes to mask his pain.
The “perfect” teen who suddenly stops eating.
This crisis wears a thousand masks—and we’re missing most of them.

Why Now? The Perfect Storm Crushing Our Kids
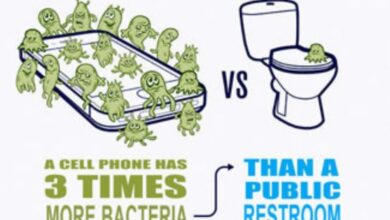
Social Media: The Double-Edged Sword
Instagram isn’t just for selfies anymore—it’s a 24/7 highlight reel that makes normal life feel inadequate.
-
Teens spending 3+ hours daily on social media have 60% higher risk of mental health issues
-
Cyberbullying victims are twice as likely to attempt suicide
But banning phones isn’t the answer. The real solution? Teaching digital resilience.
Academic Pressure Cooker
When did childhood become a race to optimize resumes?
-
AP classes x 5
-
Travel sports x 3
-
Volunteer hours x 100
No wonder burnout is the new normal for teens.
The Pandemic’s Hidden Scars
COVID didn’t just steal graduations—it stole:
✔ Social development during critical years
✔ Stability from routines
✔ Safe spaces away from troubled homes
The result? A generation with arrested coping skills.
The Warning Signs Every Parent and Teacher Must Know
Mental illness in youth rarely looks like the movies. Watch for these subtle red flags:
Emotional Changes
-
New irritability that lasts weeks
-
Loss of interest in favorite activities
-
“I’m fine” as a default answer
Behavior Shifts
-
Straight-A student suddenly failing
-
Athlete “forgetting” practice constantly
-
Drastic sleep or eating changes
Physical Clues
-
Unexplained headaches/stomachaches
-
Wearing long sleeves in summer (self-harm)
-
“Accidental” injuries that keep happening
Key Insight: Kids rarely say “I’m depressed.” They show it through what they stop doing.
Schools: The Frontline We’re Failing to Arm
The Counseling Crisis
The recommended ratio? 1 counselor per 250 students.
The reality?
-
California: 1 per 600
-
Arizona: 1 per 900
-
Minnesota: 1 per 800
We expect counselors to:
✔ Handle college applications
✔ Manage IEP meetings
✔ Prevent suicides
All while seeing each student maybe twice a year.
What Actually Works
✅ Mental health literacy in health class
✅ Teacher training to spot warning signs
✅ On-site therapists (not just guidance counselors)
Proven Example: A Maryland high school saw 40% fewer ER visits after implementing mindfulness breaks.
Families: Breaking the Stigma at Home
The Phrases That Hurt vs Help
❌ “You’re just being dramatic”
✅ “This seems really hard—tell me more”
❌ “Everyone feels stressed sometimes”
✅ “Your feelings are valid and important”
❌ “Just go to your room until you’re happy”
✅ “Let’s take a walk together”
Practical First Steps
-
Regular check-ins (not interrogations)
-
Model vulnerability (“I felt anxious today too”)
-
Know your resources (crisis lines, local therapists)
Game Changer: Families that normalize therapy see kids seek help 6x sooner.
The Lifelines That Work (When We Fund Them)
Early Intervention Programs
-
Peer support groups reduce isolation
-
Screening tools catch issues before crisis
-
Teletherapy reaches rural areas
Success Story: A Texas district’s mental health screenings led to 300% more students getting help before severe symptoms.

The Hope on the Horizon
From TikTok therapists destigmatizing care to AI screening tools in pediatric offices, innovation is fighting back.
But real change requires:
Funding mental health like we fund sports
Education starting in elementary school
❤️ Compassion replacing judgment
The kids aren’t “soft.” They’re drowning in a world we built.
And we hold the life preservers.
Read: Fungal Infections Are More Serious Than You Think: The Silent Threat Hiding in Plain Sight
Your Turn: Be Part of the Solution
-
Share this with a teacher/parent
-
Learn your local ratios (student:counselor)
-
Talk openly about mental health today